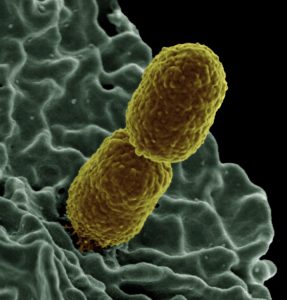
Multi-resistant bacteria are bacteria with multiple resistances against which most antibiotics have become ineffective.
Antibiotics fight bacteria and are used to treat life-threatening infectious diseases such as pneumonia. However, due to mass and improper use, more and more bacteria are becoming insensitive to many antibiotics today. Mass use also includes the administration of antibiotics to animals 1) and partly (until 2008 also in Switzerland) in agriculture. 2)
The occurrence of multi-resistant bacteria is particularly frequent and feared in the hospital environment. Hospital infections often occur in connection with a stay in a healthcare facility. According to older estimates, such infections lead to about 70,000 cases of illness and 2,000 deaths per year in Switzerland alone. In comparison, in the years 2020 – 2022 (as of May), approximately 6,335 corona deaths per year have been recorded.
The most important types
Methicillin-resistant staphylococcus aureus (MRSA). The most important transmission route for MRSA is direct transmission between people, especially via the hands. Another route of transmission is via contaminated objects, as well as from animal to human. 3.)
A distinction is made between hospital-associated MRSA, population-associated MRSA (transmission outside the hospital environment from person to person) and livestock-associated MRSA (common in livestock such as pigs, cattle and poultry; transmission from animal to human is possible).

Carbapenemase-producing enterobacteria (CPE): Multi-resistance to the antibiotics penicillins, cephalosporins, monobactams and carbapenems. Transmission with direct or indirect contact (faeco-oral). CPE is mainly transmitted through contact infection via the hands (e.g. starting from faeces and infected wounds). Resistant germs can also be transmitted to humans through contact with farm animals or from the environment of food such as fruit and vegetables. Transmission at hospitals and other health facilities is possible 4) There is an obligation to report.
Vancomycin-resistant enterococci (VRE) These are enterococci with resistance to the reserve antibiotic vancomycin. VRE can survive not only in the intestines, but also on the skin and hands of patients (and medical staff) and in the patient’s environment. Therefore, without good basic hygiene and additional transmission control measures in risk areas, they are easily transmitted from patient to patient. This risk is particularly high when patients have diarrhoea, because large amounts of the pathogens then enter the environment (nappy, bedpan, toilet, toilet seat, commode, etc.). Likewise, transmission can occur on a patient himself through contact with contaminated materials and subsequent aseptic activity.
Prevention / Measures
- Robust early detection process implemented
- Consistent admission screening for patients at risk
- Contact isolation for cases that occur
- Disinfection of the affected rooms, including documentation.
- https://www.blv.admin.ch/blv/de/home/tiere/tierarzneimittel/antibiotika.html
- https://www.agroscope.admin.ch/agroscope/de/home/themen/pflanzenbau/obstbau/feuerbrand/projekte/pflanzenschutz.html
- https://www.infektionsschutz.de/erregersteckbriefe/mrsa/#c3832
- https://so.ch/verwaltung/departement-des-innern/gesundheitsamt/kantonsaerztlicher-dienst/infektionskrankheiten/multiresistente-bakterien/carbapenemase-produzierende-enterobakterien/
- https://www.swissnoso.ch/worum-geht-es/healthcare-assoziierte-infektionen
